Endoscopies and Colonoscopies: a comprehensive overview
Colonoscopies and endoscopies are common procedures clients experience before working with me for nutrition and lifestyle coaching for gut health.
These are two incredibly important screening procedures that help us identify potential cancer, ulcer, irritation, and more. As we explore these procedures, it's imperative to critically assess their benefits against potential risks, particularly in the context of managing nuanced conditions like IBS and chronic gastritis.
Let’s take a look at these procedures:
Upper Endoscopies
What is an endoscopy, and what does it test for?
An upper endoscopy, formally known as esophagogastroduodenoscopy (EGD), is a procedure where a gastroenterologist employs a flexible endoscope to look at the upper digestive tract. This diagnostic aids in the identification and management of conditions such as acid reflux, stomach ulcers, celiac disease, and more.
What is the process like?
Preparation for an endoscopy involves careful fasting and potential adjustments to medications. During the procedure, a mild sedative ensures patient comfort. The gastroenterologist maneuvers the endoscope through the upper digestive system, capturing detailed images for examination. Basically, a tiny camera goes into your upper digestive tract to see what’s inside!
Benefits:
Endoscopies provide an unparalleled direct view of the upper digestive tract, facilitating accurate diagnosis of conditions ranging from acid reflux to tumors. The procedure also enables on-the-spot treatments, such as managing bleeding or removing polyps.
Price:
Without insurance, an upper endoscopy can cost between $1,000 to $5,000 or more, including the procedure, anesthesia, and facility fees.
Risks:
As with any medical intervention, endoscopies are not without risks. These include potential allergic reactions to sedatives, digestive tract bleeding or infection, and, albeit rarely, a tear in the digestive tract lining. It is essential to acknowledge that such complications are infrequent.
Now, let’s talk about colonoscopies.
What is a colonoscopy, and what does it test for?
Transitioning to the lower gastrointestinal landscape, a colonoscopy involves utilizing a scope to meticulously examine the colon—a gold standard for detecting colorectal cancer and various gastrointestinal anomalies.
What the process is like:
The preparation for a colonoscopy entails a comprehensive bowel washout, a procedure with potential drawbacks we’ll talk about shortly. Under general anesthesia, the doctor navigates the colon with a scope, searching for abnormalities and conducting biopsies if deemed necessary.
Benefits:
Colonoscopies are incredibly important for colorectal cancer screening, facilitating early detection and subsequently improving treatment outcomes.
Cost:
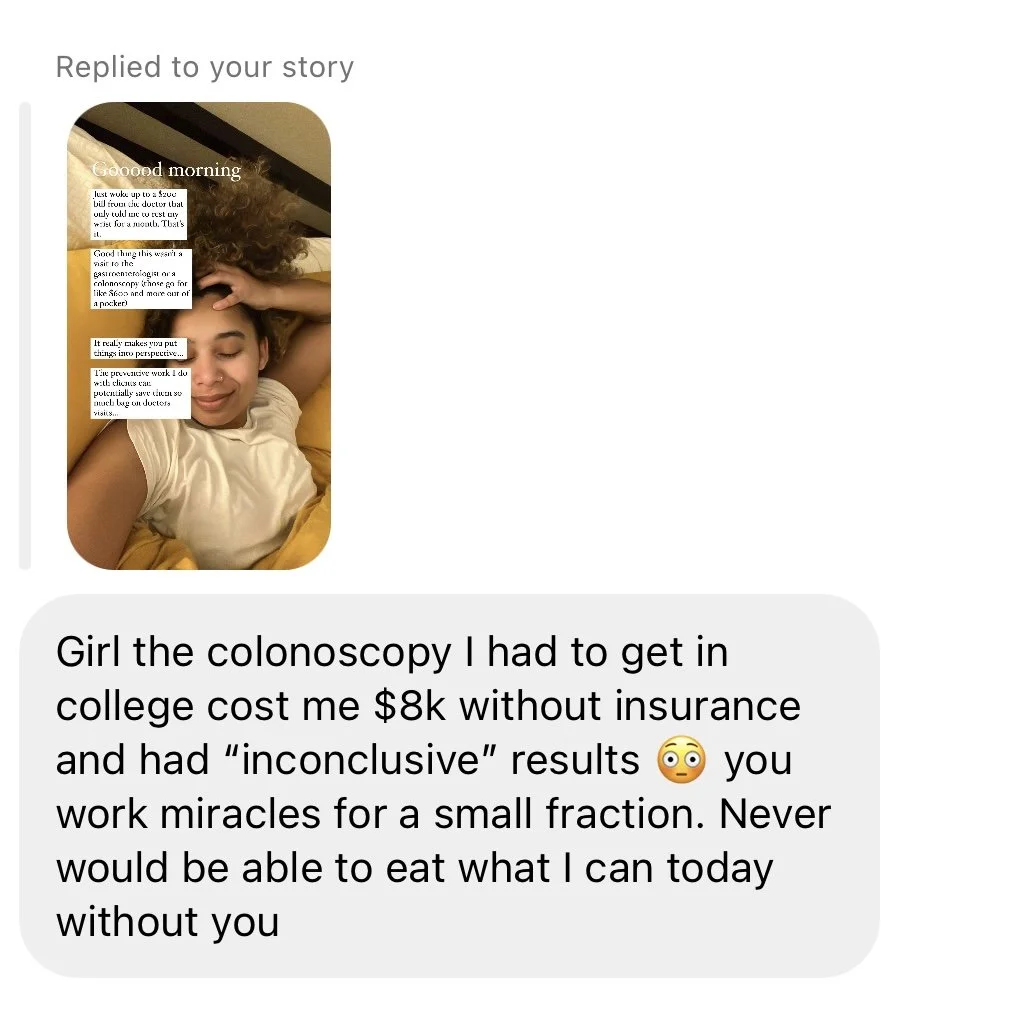
A colonoscopy can range from $800 to $3,500 without insurance. This includes the procedure itself, as well as related costs such as anesthesia and facility fees.
If you have insurance, your out-of-pocket costs will depend on your specific insurance plan. Many insurance plans cover preventive screenings, including colonoscopies, at no cost to the patient. However, if you have a high deductible or if the colonoscopy is performed for diagnostic reasons rather than preventive, you may have some out-of-pocket expenses.
Risks:
Addressing the inherent risks, albeit rare, is imperative. The foremost concern is the potential for perforation (1 in 1000 procedures), with serious complications occurring in approximately 5 out of every 1000 colonoscopies. Infections, though infrequent, are also a potential risk. Furthermore, the complete bowel washout may impact gut flora, and there is a minor risk associated with general anesthesia, according to expert physician Chris Kresser.
Are there other screening options for colorectal cancer?
Yes! See the list below:
Flexible Sigmoidoscopy:
Similar to a colonoscopy but focuses on the lower part of the colon.
It doesn't require as extensive bowel preparation, and sedation is often not needed.
Virtual Colonoscopy (CT Colonography):
A non-invasive procedure that uses a CT scanner and computer software to create detailed images of the colon.
It doesn't require sedation, but a similar bowel preparation is necessary.
Stool-based Tests:
Fecal Occult Blood Test (FOBT): Checks for hidden blood in the stool, which can be a sign of colorectal cancer or other digestive issues.
Fecal Immunochemical Test (FIT): Similar to FOBT but is more specific to human blood.
DNA Stool Test (FIT-DNA): Examines stool for DNA changes associated with colorectal cancer or precancerous polyps.
Blood Tests:
Some blood tests can help identify certain markers associated with colorectal cancer, although they are not standalone screening tools.
Capsule Endoscopy:
It involves swallowing a small capsule with a camera that takes images of the entire digestive tract as it passes through.
Double-Contrast Barium Enema:
It involves injecting barium into the colon and rectum and taking X-rays to detect abnormalities.
It's crucial to consult with a healthcare professional to determine the most appropriate screening method based on individual health factors, family history, and personal preferences. Regular screenings are essential for early detection and improved outcomes in colorectal health.
A Holistic Perspective:
While these screenings play an indispensable role in managing various gastrointestinal conditions, especifically seriously life-alterning diseases like cancer, not all of us need to restort to these procedures when we are experiencing gut issues such as constipation, diarrhea, or acid reflux. You can instead, focus on alleviating symptoms with lifestyle and dietary modifications for conditions like IBS and chronic abdominal pain. Doing this will ensure you tackle the root cause of the digestive issues, saves you money, and takes away the discomfort and the potential risks associated with conoloscopies and endoscopies.
Acknowledging the downsides of these procedures underscores the importance of weighing benefits against potential risks.
In conclusion, colonoscopies and endoscopies have a time and a place. If you are under 40 years old and with severe IBS symptoms, I suggest addressing lifestyle and diet factors with a qualified professional first. You are likely to get better and address the root cause using holistic therapies. Of course, certain risk factors might require a screening procedure earlier on, such as family history of colorectal cancer, age, and other conditions.
References:
Kresser, C. (2013, February). The Saturated Fat & Heart Disease Myth, Colonoscopy Health Risks, and Intermittent Fasting. Chris Kresser. URL: https://chriskresser.com/the-saturated-fat-heart-disease-myth-colonoscopy-health-risks-and-intermittent-fasting/
Cleveland Clinic. (n.d.). Upper Endoscopy Procedure. Retrieved December 2023, from https://my.clevelandclinic.org/health/treatments/4957-upper-endoscopy-procedure